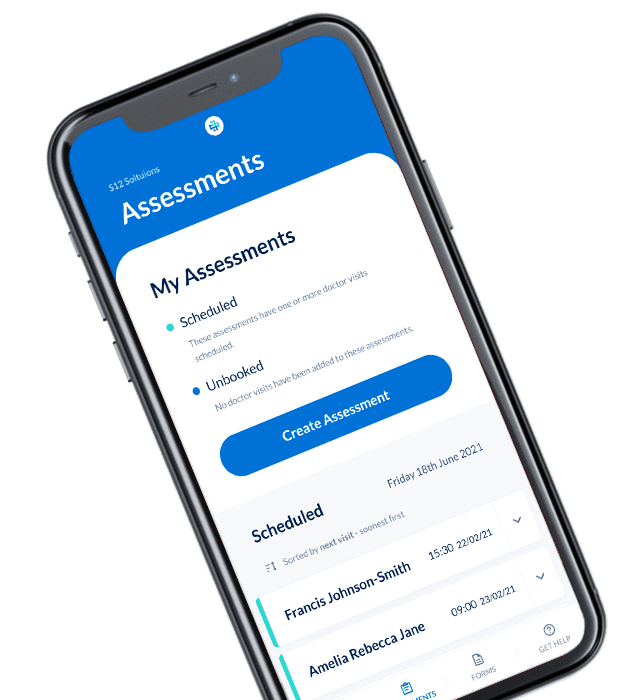
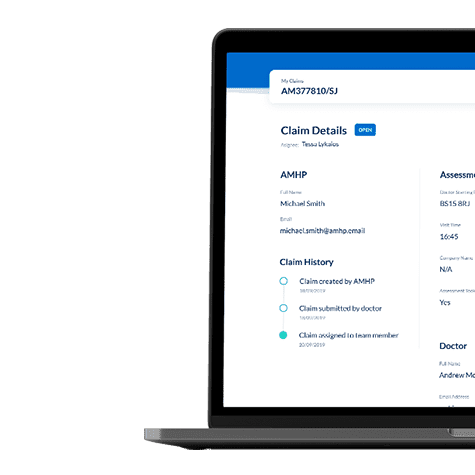
Through talking to section 12 (s.12) doctors, claim processors and other stakeholders, we learned that it is not always clear to s.12 doctors where claims should be sent or how to resolve payment problems, which in some cases was discouraging s.12 doctors from participating in s.12 work.
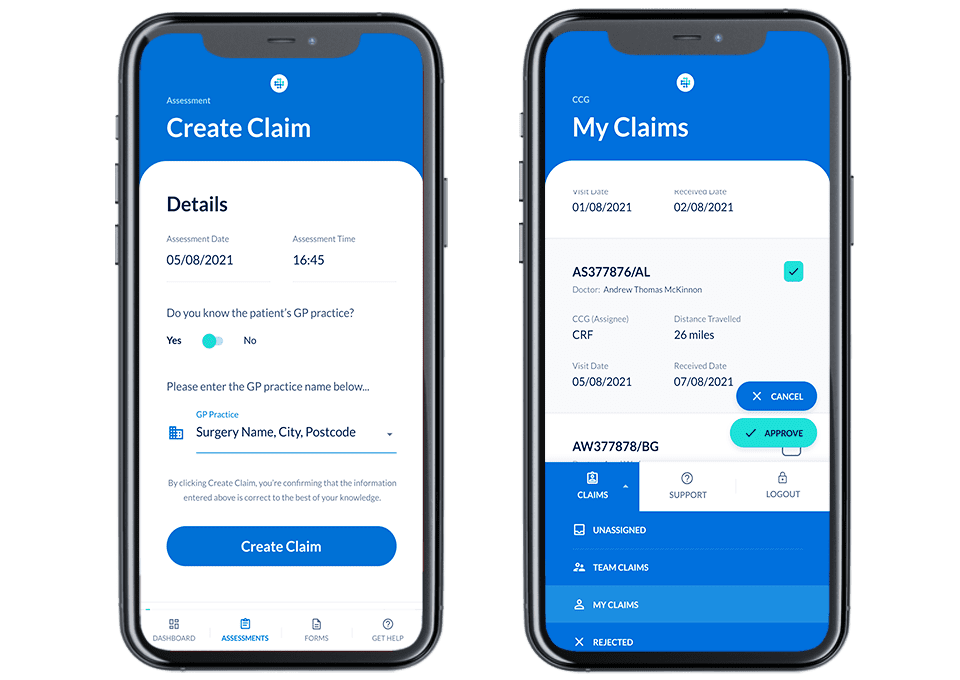
Furthermore, claim processors were routinely sent non GDPR compliant claim forms, often in bulk. Processing could be time-consuming and bulk submissions could cause problems for accountable organisations’ budgets.